|
READ: Healing complex wounds and improving patient quality of life with innovative electrical stimulation wound therapy
Wednesday, 1 December 2021
|
|
By Linda Howell, Clinical Nurse Consultant First published in WoundConnect, December 2021 The following case study is of a patient with a complex leg ulcer. As well as looking at the clinical efficacy of advanced modalities such as Accel-Heal® 12 day electrical stimulation wound therapy in improving healing outcomes, the case study considers the impact that living with a chronic wound has on patients’ wellbeing and quality of life. Accel Heal is a 12 day electrical stimulation wound therapy (Class 11A) that has been demonstrated to be effective in wound healing (Tadej et al, 2010; Taylor at al 2011). The treatment consists of six 48-hour single use units, to be applied consecutively, and electrode pads. The pre-order to modify specific functions in dermal tissue (www.accelheal.com). Treatment is delivered via electrode pads placed on the healthy skin either side of the wound. As an adjunct treatment, Accel Heal can be applied alongside the patient’s wound therapy regimen and can be used under compression bandaging. Accel Heal is now available in Australia via Alliance Medical Solutions (info@alliancemedicalsolutions.com.au). Background Mrs LK is a 67-year-old lady who is married with three children and works full time in a factory setting so is on her feet all day. She is usually an active member of her community and likes to socialise with her family and friends. Mrs LK reported the effects of living with her venous leg ulceration as “absolutely debilitating” and “the most terrible experience of my life”. She described her overall quality of life as “the worst possible” due to the physical symptoms that affected her daily life. Mrs LK experienced pain that prevented her from sleeping. She reported feeling extremely anxious and stressed as she was unable to work because of the pain and the side effects of the analgesia which made her feel very drowsy. The ulceration also impacted on her ability to perform her activities of daily living and she had to rely on her family for assistance which made her feel a “burden” to them. Over the years, a multidisciplinary team of Health Professionals had been involved:
Assessment and prior treatment Mrs LK presented to my clinic with circumferential Venous Leg Ulceration which was first identified in 2013 (8 years earlier). The wound bed was friable with some slough, tissue erosion and high levels of exudate with recurrent biofilm formation. She had repeated hospitalisations for infection and a combination of oral and IV antibiotics. A number of procedures had been carried out, including:
Mrs L reported severe pain throughout this episode of care, requiring opioid medication. There were recurrent infections (Pseudomonas, Beta Haemolytic Strep, Strep G, Staph Aureus) with odour and tissue oedema noted. Medical history Mrs LK had been diagnosed with:

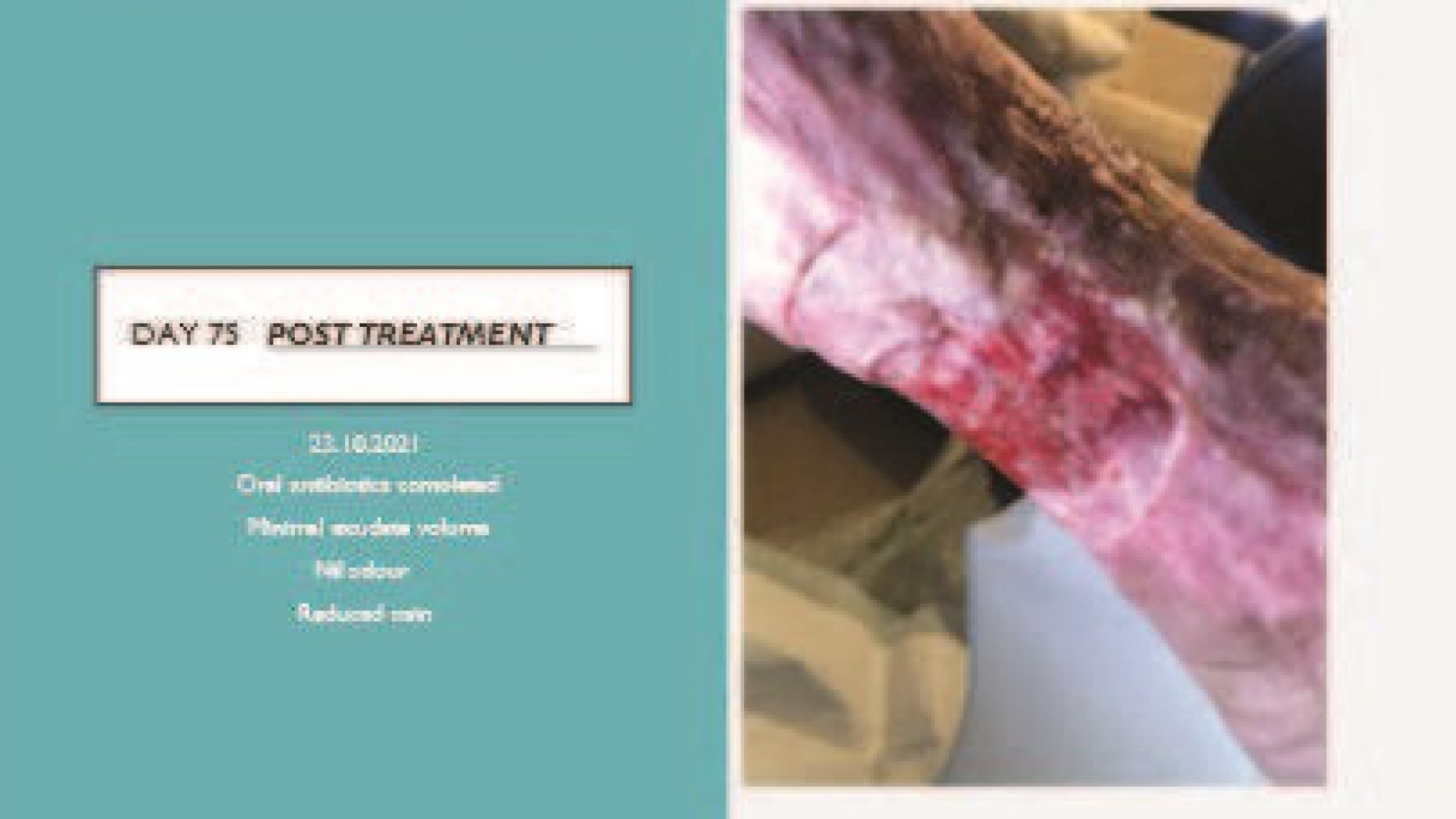
'Before', at presentation. The medial ulcer on her left leg was the original wound treated six years earlier. It was extremely painful and circumferential. 

  
 Conclusion In summary, the client was amazed and delighted at how quickly the wound improved and felt that, for the first time, she could see ‘a light at the end of the tunnel’ as far as healing her chronic wound was concerned. She looks forward to using Accel Heal on her other wounds so she can finally get back to work. • Ovens L. Electroceutical therapy to manage complex leg ulcers: A case series of three patients. Presented at: Wounds UK; 2014. Ovens L. Improving clinical ulcers ( VLUs ) using externally applied electroceutical therapy in a Community NHS Trust. In: Wounds UK. ; 2018. doi:10.1111/12
• Harvey et al 2020. Electrical stimulation for treating pressure ulcers. Cochrane Database Syst Rev.. 2020 Jan 22;1(1):CD012196 • Hofman D, Ryan TJ, Arnold F, et al. Pain in venous leg ulcers. J Wound Care. 1997;6(5):222-224. doi:10.4254/wjh.v5.i4.196 • Houghton PE. Electrical stimulation therapy to promote healing of chronic wounds: a review of reviews. Chronic Wound Care Manag Res. 2017;Volume 4:25-44. doi:10.2147/CWCMR.S101323. • Jankovi A, Bini TI. Frequency rhythmic electrical modulation system in the treatment of chronic painful leg ulcers. Arch Derma tol Res. 2008;300:377-383. doi:10.1007/s00403-008-0875-9 • Khouri C, Kotzki S, Roustit M, Blaise S, Gueyffier F, Cracowski J. Hierarchical evaluation of electrical stimulation protocols for chronic wound healing : An effect size meta-analysis. Wound Repair Regen. 2017:883-891. doi:10.1111/wrr.12594 • Koel G, Houghton PE. Electrostimulation: Current Status, Strength of Evidence Guidelines, and Meta-Analysis. Adv Wound Care. 2014;3(2):118-126. doi:10.1089/wound.2013.0448 • Lallyett C, Yeung CYC, Nielson RH, et al. Changes in S100 Proteins Identified in Healthy Skin following Electrical Stimulation: Relevance for Wound Healing. Adv Ski Wound Care. 2018;31(7):322-327. doi:10.1097/01.ASW.0000533722.06780.03 • Lallyet C, Nielson RH, Zeef L, et al. Gene expression changes in skin following microcurrent treatment. Present Collagen Gordon Res Conf. • Lo et al 2020 Int Wound J. Clinical and economic burden of wound care in the tropics: a 5-year institutional population health review. 2020 Jun;17(3):790-803. • Louison P. Management of recurrent venous leg ulcer with electro ceutical therapy * to improve pain, expedite healing and reduce risk of recurrence. Present EWMA. 2015. • Milne J, Swift A, Smith J, Martin R. Electrical stimulation for pain reduction in chronic wound healing. 2021; manuscript submitted to JOWC. • Ovens. Application of Accel-Heal® for patients with chronic venous leg ulcers: an evaluation in a community UK NHS trust. Wounds UK 2019;15(3):78–84. • Ashrafi M, Mohamed TA, Ardeshir B. The efficacy of electrical stimulation in lower extremity cutaneous wound healing : A system atic review. 2017;(August 2016):171-178. doi:10.1111/exd.13179 • Atkin L, Martin R. An audience survey of practice relating to pain in the management of chronic venous ulcers. Br J Community Nurs.2020;In Press. • Chen et al. Electric Stimulation as an Effective Adjunctive Therapy for Diabetic Foot Ulcer: A Meta-analysis of Randomized Controlled Trials. Adv Skin Wound Care: 2020;33:608–12. • Dhoonmoon P. A multi-professional approach to improve healing rates of complex patients under the care of an integrated lower limb service in an inner London Borough. Presented at EWMA 2020, Nov 2020, virtual conference. • Draper DO, Knight KL, Rigby JH. High-volt pulsed current: Treat- ment of skin wounds and musculoskeletal injuries. Int J Athl Ther • Peters et al 2001. Electric Stimulation as an Adjunct to Heal Diabetic Foot Ulcers: A Randomized Clinical TrialArch Phys Med Rehabil 2001;82:721-5. • Piaggesi A, Läuchli S, Bassetto F et al. EWMA document: advanced therapies in wound management: cell and tissue based therapies, physical and bio-physical therapies smart and IT based technologies J Wound Care, 2018; 27(6), Suppl 6. • Posnett et al. 2020. Cost-effectiveness of a single-use, portable electrical stimulation device in the management of venous leg ulcers. Presented at EWMA 2020 (virtual meeting). • Turner and Ovens. 2018. Clinical outcome results and quality of life improvements using electroceutical treatment * - Patient perspectives. In: EWMA 2018. ; 2018. • Wounds UK (2019) Accel-Heal® electrical stimulation Made Easy. London: Wounds UK. Available from: www.wounds-uk.com/made-easy. • www.infinityrehab.com/files/2015/02/Improving-Clinical-Out comes-Utilization-of-Electrotherapy-Diathermy-and-LASER-power point.pdf Accessed August |
